
Fitness professionals, such as athletic trainers, strength and conditioning coaches, and personal trainers, with athletes for clients, serve on what may be considered the frontline of sports medicine. Because of the extensive amount of time they spend with athletes, they may be the first to hear of an athlete’s new symptoms. Although these symptoms often may be indicative of a sports injury, it is prudent to consider that many medical conditions can mimic the symptoms of various sports injuries because both medical problems and sports injuries can present similarly with pain. An attempt at diagnosis without appreciating the full breadth of the possible diagnoses may delay effective treatment and can have undesirable consequences.
A 19-year-old college baseball catcher experienced left lateral knee pain when going into his squat. His athletic trainer diagnosed iliotibial band syndrome andtreated him with strengthening, stretching, and ultrasound. The athlete did not improve, so the trainer advised him to rest for the summer. After transferring schools, the athlete developed pain on the first day of baseball practice. At this point, 11 months had elapsed since his pain first appeared. His new trainer sought medical consultation within his sports medicine team. The examination disclosed difficulty duck walking and tenderness, swelling, and crepitus with motion at the lateral femoral condyle.

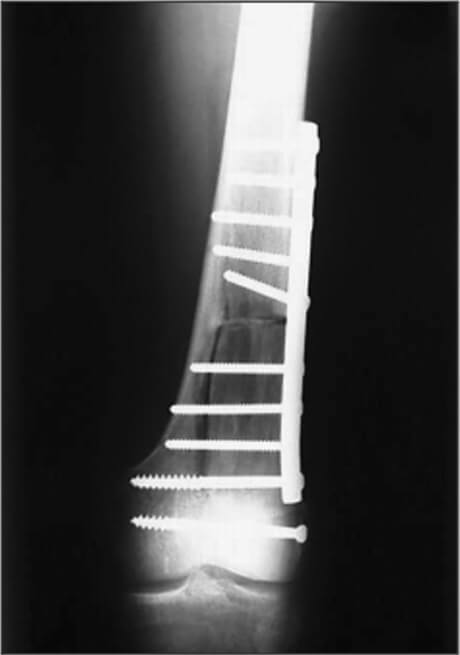
Plain X-rays revealed a lytic lesion in the lateral femoral condyle (Fig. 1). Biopsy demonstrated the tumor to be a fibrosarcoma, and the patient was treated with replacement of his lateral femoral condyle from a cadaver source (Fig. 2).

Although the diagnosis in this case is a rare type of malignancy, the athlete’s presentation illustrates how common and reassuring the symptoms can be in the presence of a serious disease. The athlete’s symptoms were clearly reassuring to his first trainer, who remained sure of his initial diagnosis, even after the athlete’s failure to improve.The second trainer was part of awell-established sports medicine team, in which physicians made weekly visits to the training room and a collaborative relationship existed between team members.
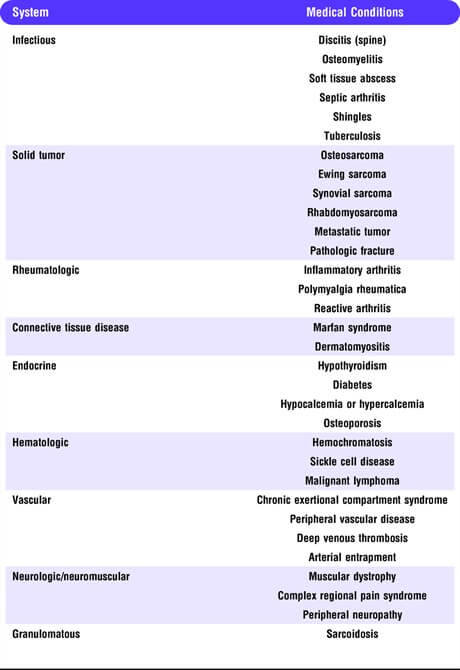
Accurate diagnosis begins with consideration of the list of possible diagnoses for the patient’s symptoms, known as the differential diagnoses. Differential diagnoses, because of their scope and level of detail, are difficult to master. It is impossible to memorize an exhaustive differential for every symptom presentation. One should be taught, instead, to think in terms of systems. Table 1 presents a systems approach to medical conditions that may mimic sports medicine conditions. Note that this list is not comprehensive. For example, there are many bone tumors not listed, and some medical conditions, such as tuberculosis and sarcoidosis, are capable of mimicking just about any other condition because of the wide variety of types of tissues that they can affect.
Diseases of the organs of the chest, abdomen, and pelvis may present in a manner suggestive of a musculoskeletal(MSK) condition. Visceral (internal organ) pain referral patterns may include shoulders, the entire spinal axis, and hips(2,4). Table 2 lists a differential diagnosis for low-back pain, and it contains some examples of internal organ derangements. The low back also is a frequent site of pain in sickle cell disease (3). It is important to note that disorders of internal organs can present atypically, for example, a gastrointestinal (GI) disorder producing hip pain only and no GI symptoms.

The differential diagnosis of shoulder pain also is extensive. Interestingly, shoulder pain can be the sole presenting symptom of Parkinson’s disease (PD)and can remain so for the first few years of the disease. In a review of 82 patients with PD, 33% had presented with MSK pain that was attributed to an MSK disorder, such as arthritis or frozen shoulder. After beginning pharmacotherapy for PD, typically years after its initial presentation, 85% of patients in this group experienced an improvement in their MSK pain (1).
The shoulder is often a site of referred pain from a visceral source, such as from coronary artery disease, an injury to the spleen or liver, or from a disorder within the apex of the lung (e.g., Pancoast tumor). Frozen shoulder is a common MSK problem, but it may occasionally signal the presence of organic disease. It is frequent in diabetics, and it may occur as a consequence of a malignancy (5,6) or in heart disease.
In addition to pain syndromes, exercise professionals may encounter medical conditions that are specifically associated with exercise, such as heat illness, certain cardiac conditions, exercise-induced GI symptoms, overtraining syndrome, and exercise-induced asthma. A hasty attempt at diagnosis in these situations, without consideration of the scope of the differential diagnosis, serves the patient poorly, just as it does with pain syndromes. The differential diagnosis of overtraining syndrome, for example, is the same as that of chronic fatigue and is therefore complex. Exercise-induced collapse in the heat may indeed be caused by heat stroke, but cardiac causes, cerebrovascular accident (stroke), and hyponatremia also must be considered. Failure to diagnose such a condition correctly and promptly may lead to poor outcomes.
Attempting diagnosis without knowledge of the medical mimics of sports medicine conditions means that the would-be diagnostician is operating with an incomplete differential diagnosis. It is therefore desirable that fitness professionals use a team approach, in which they have easy access to a physician trained in both MSK and medical conditions. A collaborative relationship is beneficial for all team members and also serves to help the team develop guidelines for when an athlete should be referred to the physician. Case discussions among team members should be encouraged because they help fitness professionals to develop a sense of when cases are atypical and perhaps more serious. Such discussions also help the physician members of the team broaden their perspectives and appreciate the capabilities of other team members.
The case presented above consisted of a rare malignant bone tumor. Although it is important to consider the possibility of a rare and serious disease when an athlete presents with new onset of pain, it is more important to realize that the differential diagnosis for any symptom consists of disorders involving multiple systems. We should always includenon-MSK items in our differential diagnoses.
This will ensure that the history and examination are more complete and will allow more flexibility on the part of the diagnostician if the initial diagnosis turns out to be incorrect.

1. Farnikova K, Krobot A, Kanovsky P. Musculoskeletal problems as an initial manifestation of Parkinson’s disease: a retrospective study. J Neurol Sci. 2012; 319 (1–2): 102–4.
2. 2. Giamberadino MA, et al.Handbook of Clinical Neurology: Pain. Cervero F, Jensen TS, editors. Amsterdam, Netherlands: Elsevier BV; 2006;81:343.
3. McClish DK, Smith WR, Dahman BA, et al. Pain site frequency and location in sickle cell disease: the PiSCES project. Pain. 2009; 145 (1–2): 246–51.
4. Perry CP. Pelvic Pain: Diagnosis and Management, Howard FM, editor, Philadephia (PA): Lippincott, Williams and Wilkins; 2000, p. 485.
5. Robinson D, Halperin N, Agar G, et al. Shoulder girdle neoplasms mimicking frozen shoulder syndrome. J Shoulder Elbow Surg. 2003; 12 (5): 451–55.
6. Sano H, Hatori M, Mitsuyoshi M, et al. Tumors masked as frozen shoulder: a retrospective analysis. J Shoulder Elbow Surg. 2010; 19: 262–66.